What you need to know about winter allergies
There’s a lot to love about winter — sweater weather, holiday parties, snowy outdoor activities, and a break from typical allergies caused by things like pollen that are common in the spring, summer, and fall.
Unfortunately for some, this change in seasons may also trigger new allergic reactions or cold weather allergies.
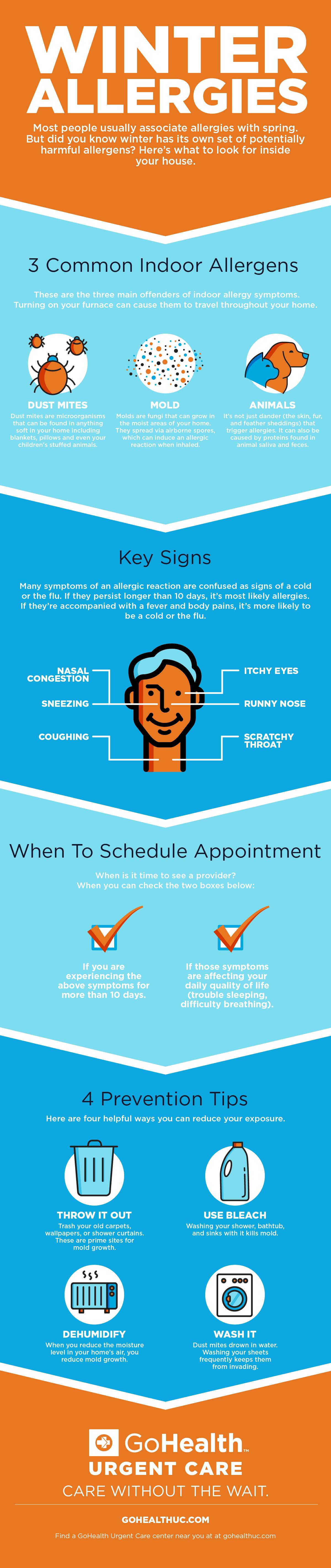
The main difference between a cold weather allergy and other seasonal allergies is that allergies in winter are more dependent on your lifestyle than on your outside environment. In other words, since you’re not going outside as much and plants aren’t blooming in the winter, allergies are triggered by the accumulation of indoor irritants. This means winter allergies are most often caused by mold and dust mites, as our exposure is increased when we spend more time indoors.
Winter allergy symptoms
The symptoms of winter allergies are similar to the flu or a cold. However, if those symptoms last more than a week to ten days, allergies are probably to blame. The more prolonged your symptoms are, the more likely they’re related.
If your symptoms come with a fever, cough, aches, and pains, it’s more likely a cold or the flu. Airborne allergens do not cause a fever and are much less likely to cause body aches or a sore throat. Chest pressure is more likely when you’re sick, but if you have asthma, this could be a symptom of an allergic reaction, too.
Below are some common allergy symptoms in the winter:
- Coughing
- Itchy eyes
- Nasal congestion
- Runny nose
- Scratchy throat
- Sneezing
While colds will resolve on their own, allergies may only resolve when the weather changes and you can spend more time outside and less time indoors.
Types of winter allergens
When you turn on your furnace to warm up the house, indoor winter allergens become airborne, accelerating your exposure to them and triggering allergens. While these allergens are present year-round, your exposure to them is lower in the warmer seasons.
Dust mites
Dust mites are microscopic bugs that live in household dust. They are close relatives of ticks and spiders. They eat skin cells shed by humans and thrive in warm, humid environments like homes. They can be found in anything soft around the house, including blankets, pillows, and even children’s stuffed animals.
Mold
A fungus that grows inside your home, mold often lurks in dark, damp spaces like basements and bathrooms. Mold is attracted to moist places, and breathing it can cause an allergic reaction for many people who spend more time inside in the winter.
Animals
Dog and cat allergies are not triggered by pet fur but rather by a protein in animal skin cells, saliva, and urine. Your pet’s hair isn’t an allergen, but pets can bring in other allergens from outside or around the house on their fur.
Itchy feet
Itchy feet in the winter could result from dry household environments and exposure to irritants when walking around barefoot. Infectious germs like bacteria, fungi, parasites, or viruses can cause itchy feet. Feet doesn’t have oil glands, so the combination of low humidity, hotter showers, lack of moisture, and dry winter air can cause red, itchy skin that peels or cracks.
Treatment for allergies in winter
If you suffer from winter allergies, you know they can greatly interfere with your day-to-day activities, especially because the symptoms last longer than the average cold.
Treatment can depend on the severity and symptoms that you’re experiencing. Some of these may include:
- Asthma treatment: If you have asthma and experience severe cold weather allergies, treatments like an inhaler may be beneficial.
- Decongestants: Decongestants may also be used to clear mucus and relieve congestion and swelling.
- For itchy feet: If you have itchy feet in the winter, try adding daily moisturizer and sleeping with socks overnight to keep lotion in place. Lower the temperature of your bath water, stay hydrated, use a humidifier, gently exfoliate the skin, and allow your feet to breathe.
- Immunotherapy: If you’re regularly experiencing allergic reactions, immunotherapy in the form of allergy shots may be a good idea to speak with your healthcare provider about.
- Medication: Over-the-counter antihistamines, nasal steroids, and prescriptions can help target some allergy symptoms.
- Nasal rinses: Using nasal sprays or a neti pot to rinse your nasal cavity can help keep your passages clear and reduce the severity of allergy reactions.
While these treatments can provide some symptom relief, certain preventive practices are also important for winter allergy sufferers.
Prevention for winter allergies
Winter allergies are not entirely preventable. However, if you know you’re sensitive to certain types of allergens, you can take steps to avoid a reaction or reduce the severity of one.
- Combat dust mites: Do this by using a HEPA air filter, washing bedding in hot water (130 F) weekly, and using allergy-proof covers on mattresses, pillows, and comforters.
- Control pet allergies: If you don’t have a pet but want one, consider adopting hairless animals like goldfish. If your life isn’t complete without a cat or dog, don’t let it sleep in your bedroom (if you can help it!), and give it a bath at least once a week.
If you’re visiting friends or relatives with furry friends, take allergy medication beforehand, and bring your own pillow and blanket if you are staying overnight.
- Reduce mold: Wage war on mold by throwing out shower curtains, wallpaper, and carpeting that have it, washing showers and sinks with a solution containing 5% bleach and detergent, and using a dehumidifier to keep the humidity in your home below 50%.
These lifestyle changes can help reduce the severity of allergies in the winter, helping improve your symptoms during the colder months.
Winter allergies FAQ
Here are some frequently asked questions about cold weather allergies:
What is the difference between allergies and the common cold?
Colds are triggered by a virus spread through contact, whereas allergies are triggered by exposure to an irritant that produces a histamine reaction in your body.
Why do I have allergies in the winter?
Allergies in the winter are caused by increased exposure to indoor allergens, such as dust or mold. In the warmer months, we may spend more time outdoors, reducing our exposure to these irritants. Therefore we might not struggle with these types of allergies as much.
What are indoor allergy symptoms?
Indoor allergy symptoms are similar to any allergy symptoms. Typically, you might experience a runny nose, sneezing, itchy eyes, and cough.
Can hay fever happen in winter?
Hay fever is another common name for allergies, which can happen at any time of the year.
Does humidity affect allergies?
Yes, humidity can increase the presence of certain allergens in your home, particularly dust mites and mold. If cleaned and maintained properly, a humidifier can help reduce allergy symptoms.
When to visit urgent care for winter allergies
If you’re experiencing symptoms like itchiness, sneezing, coughing, and congestion for more than a week or two, or they’re affecting your daily quality of life, it’s probably time to see a healthcare provider to confirm allergies and establish a longer-term plan.
We have knowledgeable providers ready 365 days a year to assist you at any time. Our goal is to help you get your allergies under control so that you can go back to enjoying all the cozy perks winter has to offer.
Our providers can help you find immediate relief through a combination of medication and lifestyle changes. Further allergy management may require a referral to an allergist, who can perform a skin test that checks your reaction to specific allergens. When you know what you’re allergic to, you can minimize your exposure and get back to feeling better. Our vast network of partners can help you find the best allergist to meet your needs.
If you need help assessing and treating winter allergies, visit the experts at one of our urgent care locations. You can walk in without an appointment or save your spot online. We are open 365 days a year, even during the winter holidays. We will have you back to feeling better in no time.
Medically reviewed by J.D Zipkin, MD, MA, FAAP — By Sarah Thebarge, Physician Assistant on December 26th, 2023


